European Society of Cardiology (ESC) Clinical Consensus Statement on Obesity and Cardiovascular Disease
- Obesity affects about one in eight adults worldwide.
- The prevalence of obesity has been rising over the past decades globally.
- While marked obesity (BMI ≥35 kg/m2) is an emerging phenotype, most cases of obesity-related CVD are expected to arise from persons with BMI <35 kg/m2.
- Preventive measures should focus particularly on childhood and early adulthood and address socioeconomic disparities.
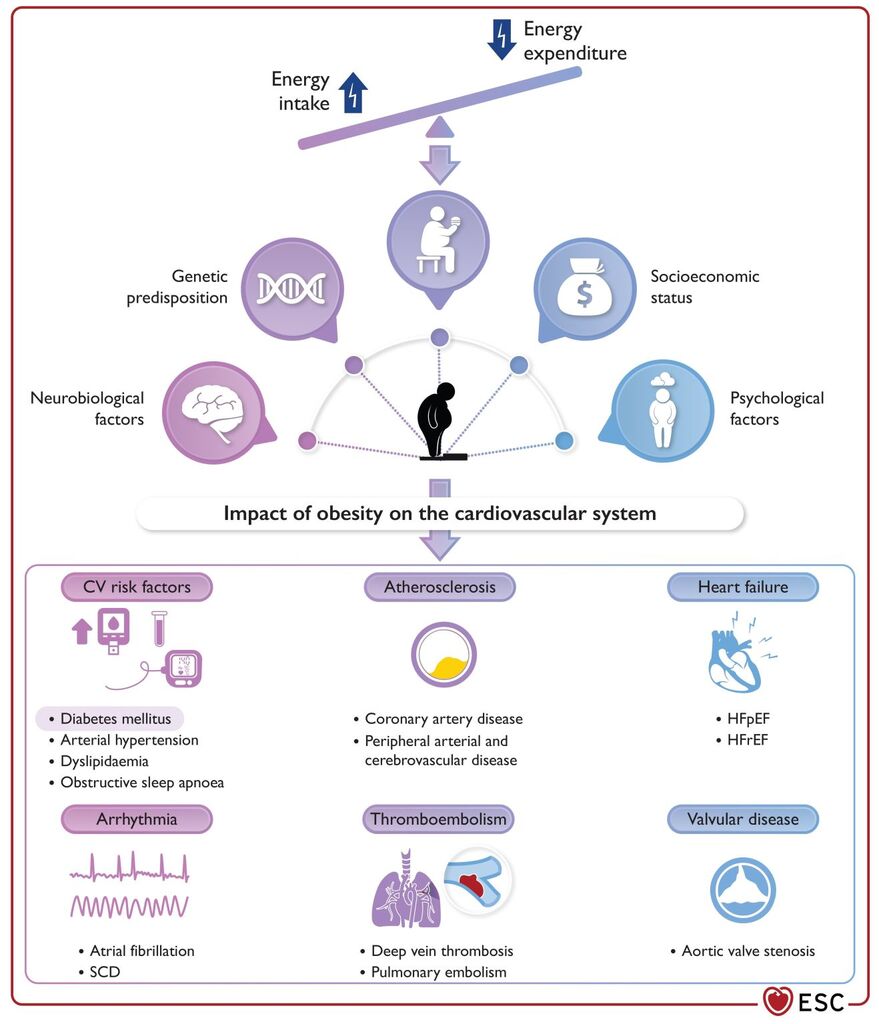
- Genetic and biological factors influence individual development of obesity, but the worldwide obesity epidemic is largely driven by environmental/societal factors.
- Individuals with similar BMI may have different cardiometabolic risks.
- Metrics of abdominal adiposity including waist circumference, waist-to-height ratio and waist-to-hip ratio are useful to refine cardiometabolic risk stratification beyond BMI.
- Different imaging modalities can accurately assess fat topography and quality.
- Quantification of perivascular, epicardial, and pericardial adipose tissue may improve CV risk assessment, but its clinical role remains uncertain.
- Remote and local adipose tissue exert pro-atherogenic and pro-inflammatory effects on coronary vascular wall and myocardium, but may also shift to anti-atherogenic effects.
- Overweight and obese individuals should regularly be screened for T2DM, particularly after age 45.
- In patients with obesity and T2DM, hypertension, dyslipidemia, or OSA, reducing weight is a cornerstone of treatment.
- Dietary interventions generally aim for a 500–750 kcal/day energy deficit. Adjustments to individual body weight and activity are needed.
- Weight reduction in the range of 5%–10% can be achieved with various nutritional and multidisciplinary approaches but maintenance of effects is a key issue.
- Physical activity interventions typically have modest effects on weight loss but are important for weight loss maintenance and reduction of overall CV risk.
- GLP-1RAs are effective for weight loss and improvement in CV risk factors.
- Currently, the only weight loss intervention with proven outcomes in patients with established CVD without T2DM is semaglutide 2.4 mg/weekly.
- Treatment effects are limited to the duration of treatment. The long-term effects and maintenance of efficacy of weight loss medications requires further investigation.
- Bariatric surgery should be considered for obese high-risk individuals when lifestyle change does not result in maintained weight loss (Class IIa, level of evidence B).
- Bariatric surgery should be considered for high and very high-risk patients with T2DM and BMI ≥35 kg/m2 when repetitive and structured efforts of lifestyle changes combined with weight-reducing medications do not result in maintained weight loss (Class IIa, level of evidence B).
Read also:
Read also: Dr. Suzan Gharaibeh

